Group Chat Mothers’ Meeting Leads To HPV Vaccine Scare
Cervical cancer related deaths are set to double in the Middle East by 2035. Conservative nations are encouraged to vaccinate people against HPV and tackle sexual taboos. The Ministry of Health and Prevention added the HPV vaccine to the National Immunisation Programme for the first time in the Northern Emirates this year.
The HPV vaccine provides protection against different types of the Human Papilloma Virus, which causes the most cases of cervical cancer. Cervical cancer is the second largest cancer killer of women in the Middle East and North Africa regions. However, doctors are saying the spread of misinformation amongst some mothers is causing confusion and unnecessary worries about the HPV vaccine.
Dr Abo Hamed, who has been dealing with the misunderstandings around the HPV vaccine, said:
“I explained to the mothers who received the messages that the vaccine is given through the muscle, preferably in the shoulder, like any other vaccine, and it does not have any negative effects on their daughter’s health, their immune system or their productivity in future.”
She goes on to discuss the importance of the HPV vaccine, saying: “it is a very important step in the primary prevention of cervical cancer as it prevents the infection from happening in the first place, which in turn protects the girls from developing cervical cancer.
Mike Asher, CEO and Chairman of Better2Know, says:
“Getting vaccinated against HPV is the only measure available today that will cut your risk of HPV induced cancer or genital warts. Getting vaccinated is quick, easy, pain free and might just save your life”
What is cervical cancer?
Cervical cancer is a condition that develops in the lining of a woman’s cervix. This is the entrance to the womb from the vagina. This condition occurs when the cells in the cervix start to grow out of control. These cells can then invade nearby tissues and spread throughout the body.
Stages of cervical cancer
Cervical cancer often develops gradually. The condition starts with a pre-cancerous condition known as dysplasia. This is the term for abnormal cells that are not cancerous but have the potential to become cancer. It can take years for the abnormal cells to turn into cervical cancer.
Stage 1: A small amount of cancer is found in the tissues of your cervix. These can only be seen when using a microscope.
Stage 2: Cancerous cells have spread passed your cervix. However, the cancer has not reached your pelvic wall or the lower third of your vagina.
Stage 3: The cancer has spread to the lower third part of your vagina, or your pelvic wall or you are experiencing kidney problems. Alternatively, it may have triggered all of these circumstances.
Stage 4: The cancer cells have reached your bladder, rectum, or other parts of the body.
Causes of cervical cancer
The Human Papilloma Virus (HPV) causes most cases of cervical cancer. This common viral infection is spread through unprotected sexual contact, including vaginal, anal and oral sex. There are many different types of HPV.
Some HPV strains can cause cervical cancer, most commonly high-risk types 16 and 18. Other types of HPV cause genital warts, usually low-risk types 6 and 11. Warts are growths around the genital area that can be passed on through skin-to-skin contact alone. Genital warts affect both men and women. You are at high risk of catching them if you have unprotected sex with someone who has genital warts.
The HPV vaccine will protect you against these strains of the virus.
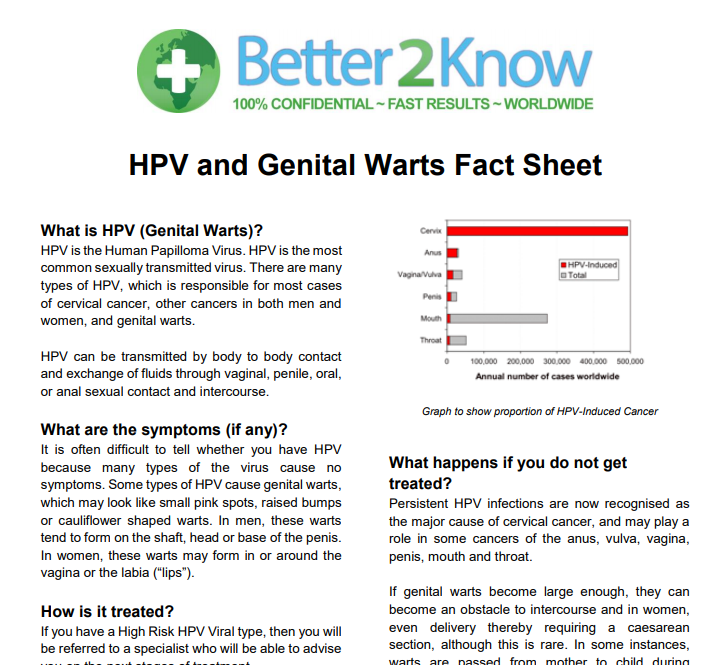
Find out more with Better2Know’s HPV and Genital Warts Factsheet
The HPV vaccine
HPV prevalence in the Middle East and North Africa regions present a public health issue. The HPV vaccine will protect you against various types of the virus. The World Health Organisation (WHO) recommends males and females are both vaccinated, particularly between the ages of 21 and 26.
The acceptance of the HPV vaccine in the Middle East remains controversial. However, getting vaccinated against HPV remains the most effective way to prevent infection and to help decrease cases of cervical cancer and genital warts.
The HPV vaccine is administered to your upper arm or thigh. Three doses of the vaccine are needed to fully protect you. The second dose will be administered one to two months after your first dose. The third dose will be given 6 to 12 months after your first dose. If you are experiencing any signs of ill health, or have been allergic to vaccines in the past, your HPV vaccination may be postponed.
Cervical cancer symptoms
Symptoms of cervical cancer are not usually present until the later stages of infection. Signs of a cervical cancer infection can include:
- Pelvic pain
- Unusual vaginal discharge (pale, watery, pink, brown, bloody, or foul-smelling)
- Pain during vaginal sex
- Abnormal vaginal bleeding
As mentioned above, cervical cancer symptoms are not often exhibited until the disease has reached an advanced stage. Therefore, it is important to receive regular cervical screening, as well as HPV testing. This ensures you will know of any cell changes earlier, enabling you to receive treatment earlier, which could help prevent the development of cervical cancer.
Cervical cancer testing
You can test for cervical cancer by having a pap test (cervical smear test) with your doctor or at a sexual health clinic. Your smear test will detect abnormal changes in the cells lining your cervix. Your doctor will take a small sample of cells from your cervix and send them to a laboratory for testing. If abnormal cell changes are detected, you will be referred for further testing.
Two days before your cervical cancer test, you are advised to refrain from:
- Using tampons
- Having sex
- Douching
- Using vaginal creams or medicines
- Using vaginal deodorant powders or sprays
Dr Gina Ogilvie, a professor and Tier 1 Canada Research Chair in Global Control of HPV-related diseases and prevention at the University of British Columbia, said:
“There has been a significant body of evidence that shows that by including HPV testing — as co-testing with cytology — we could improve detection of precancerous lesions of the cervix.”
An HPV test will detect various types of HPV. A swab sample of the cells lining your cervix will also be taken for this testing option. If you test positive for HPV, further testing will be done.
Cervical cancer risk factors
Most cases of cervical cancer are caused by HPV. This virus is an STI that is passed on through sexual contact. You can catch HPV through touch alone. Therefore, you should make sure to get vaccinated against HPV. It is also important to ensure you use protection whenever you are engaging in sexual activities.
Circumstances that may increase your chances of developing cervical cancer:
- Having HIV or any other condition that weakens your immune system
- Smoking
- Taking birth control pills for a long time
- Giving birth to three children or more
Sources
[1] CNN: HPV test more effective than Pap smear in cancer screening, study suggests
[2] Department of Health Abu Dhabi: Stages of Cervical Cancer
[3] Department of Health Abu Dhabi: Screening and Early Detection
[4] Department of Health Abu Dhabi: What is cervical cancer
[5] Emirates Woman: Here’s why you need to get screened for cervical cancer
[6] Journal of Epidemiology and Global Health: The impact of teachings on sexuality in Islam on HPV vaccine acceptability in the Middle East and North Africa region
[7] National Cancer Institute (NCI): NCI Dictionary of Cancer Terms – Dysplasia
[8] Nature Asia: Finding acceptance for a life-saving vaccine in the Arab region
[9] NHS: Cervical cancer
[10] NHS: Cervical Screening
[11] The National: Mothers consider opting daughters out of HPV vaccine over fears it causes infertility
[12] Reuters: Cervical cancer to double across Middle East without vaccines
[13] Vein Cure Clinic: Warts (Genital and Non-Genital)
Categories
- Abu Dhabi
- Bacterial Vaginosis
- Bahrain
- Blood Tests
- Cancer
- Cervical Cancer
- Chlamydia
- Dubai
- Fertility
- Gardnerella
- Genital Warts
- Gonorrhoea
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Herpes
- HIV (AIDS)
- HIV Testing
- HPV
- Instant Testing
- Kuwait
- Locations
- Middle East
- Mycoplasma
- Oman
- PAP Smear
- Positive STI Results
- Qatar
- Saudi Arabia
- Sex Education
- Sexual Health
- Sexual Health News
- Sexually Transmitted Infections
- STD Symptoms
- STD Tests and Screens
- STI Results
- STI Treatment
- STIs
- Sustainability
- Swab Tests
- Syphilis
- Trichomoniasis
- Uncategorized
- United Arab Emirates
- Ureaplasma
- Urine Tests




