What STIs can cause vaginal sores?
No one wants to find a sore on their genitals.
When it happens, it can be a serious cause for concern. After all, developing sores, bumps, or lesions around the vagina can signify the presence of a sexually transmitted infection (STI).
However, if you’ve discovered a sore on your vagina, it’s important to understand what it may be and the kind of treatment you should seek.
In this blog post, we’ll explore what vaginal sores are, what STIs are known to cause them, and how to move forward if you notice any strange bumps or lesions in your genital area.

What are STIs?
STIs, sometimes also known as sexually transmitted diseases (STDs), are infections that usually spread from person to person through sexual intercourse, including vaginal, anal, oral sex, and other forms of sexual contact.
However, many STIs can spread in other ways, like through skin-to-skin contact, sharing needles for injecting drugs, or blood transfusions.
While many of these infections can cause visible symptoms, most STIs are asymptomatic. In some instances, infections may cause symptoms that some may ignore as insignificant or confuse for the symptoms of other infections.
This is what makes many STIs so pernicious and difficult to detect.
What is a vaginal sore?
A vaginal sore means that there is an area where the top layer of skin is missing and open to the outside world in or around the vagina.
Vaginal sores may come in many forms – they can be painless or painful, singular or occurring in clusters, starting off as being fluid-filled or hardened bumps.
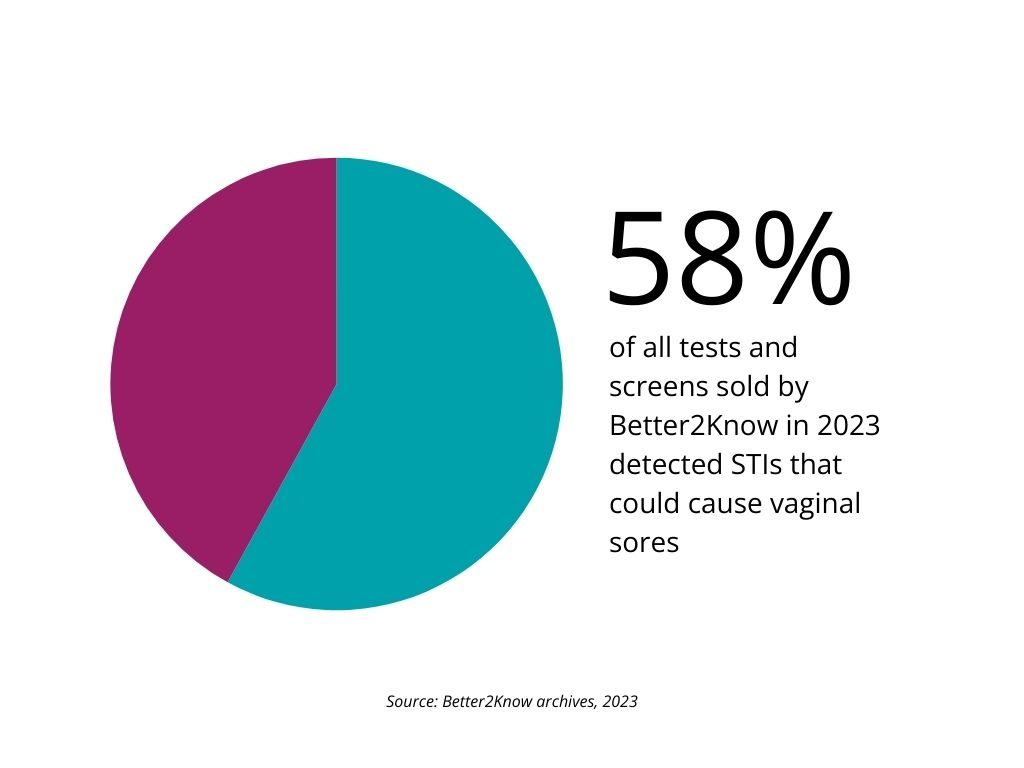
Genital sores are nothing to be ashamed of, and are quite common. At our clinics in the Middle East, 58% of all tests and screens sold by Better2Know detected STIs that could cause vaginal sores.
Worried about STIs? Get tested at a Better2Know clinic today.
What STIs cause vaginal sores?
Several sexually transmitted infections are known to produce sores, bumps, or lesions in the vaginal area. Here are some of the most common culprits.
Syphilis
Syphilis is a highly contagious STI caused by the bacteria Treponema pallidum. It progresses through four distinct stages: primary, secondary, latent, and tertiary.
During the primary stage, many people develop a small, painless genital sore called a chancre.
These red, round chancres typically appear on or around the vagina about 10−90 days (21 days on average) after the initial infection. The chancre lasts between 3 to 6 weeks before going away on its own.
However, because the sore of primary Syphilis doesn’t hurt, if it has occurred in a part of your body you can’t see (further inside your vagina, in your rectum or throat) you will probably not even know you have the infection.
When a chancre appears on an infected person, it is highly infectious and can spread the bacteria through direct contact. If the infected person doesn’t receive treatment, they will continue to be infectious.
Some people don’t get tested when these see the sore and then feel relieved that it has disappeared. But if left untreated, the Syphilis infection will become latent and spread. Over time, it will affect many of the body’s organ systems, including the brain, heart, eyes, bones, and blood vessels. The infection can be fatal. However getting tested is easy, and Syphilis is easily treatable with antibiotics.
Herpes
Herpes Simplex Viruses, namely HSV-1 and HSV-2, are infamous for causing recurrent outbreaks of painful cold sores and genital sores.
HSV-2 is most associated with Genital Herpes (although it is possible to get an HSV-1 infection in the genitals). Occasionally, the virus may be present with no visible signs and can still be passed on by a process called ‘asymptomatic shedding’.
When infected with Genital Herpes, most people initially experience a severe outbreak with many fluid-filled blisters that eventually burst and form painful genital ulcers. These sores can appear on and around the vagina, cervix, vulva and anus, and are often preceded by other symptoms like fever, body aches, and swollen lymph nodes.
The first episode or outbreak is usually the most severe, with later outbreaks becoming milder and less frequent over time. Recurrent outbreaks tend to involve fewer sores that heal more rapidly but can still be very uncomfortable.
Other causes of vaginal sores
The human papillomavirus (HPV), the most common STI, can cause protrusions of the skin in and around the genitals. These protrusions are called Genital Warts.
These warts can appear as single or clustered growths in and around the vaginal area. They can be raised, flat, or cauliflower-shaped. The colour of these warts can vary from person to person. Low and high-risk HPV can be spread through sex, but also through simple skin-to-skin contact with an infected person’s genitals or warts.
Genital Warts are usually painless, though they may itch, bleed, or cause discomfort depending on their location.
Several strains of HPV can lead to precancerous changes in the cervix. For this reason, routine HPV tests and PAP smears are recommended to detect any abnormal cervical cells before they potentially become cancerous.
Final thoughts
If you’ve noticed any bumps, sores, or lesions around your vagina, don’t panic. They may be benign, or they may represent something more serious. The best way to know for sure that your symptoms are not due to an STI is to get tested.
At Better2Know, we provide private, confidential and affordable STI testing services.
Book online today to secure your confidential STI test with one of our conveniently located clinics. Call the number at the top of this page if you need help booking your appointment.
This blog has been medically reviewed by Dr. Steve Chapman, 02/10/2024.
Categories
- Abu Dhabi
- Bacterial Vaginosis
- Bahrain
- Blood Tests
- Cancer
- Cervical Cancer
- Chlamydia
- Dubai
- Fertility
- Gardnerella
- Genital Warts
- Gonorrhoea
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Herpes
- HIV (AIDS)
- HIV Testing
- HPV
- Instant Testing
- Kuwait
- Locations
- Middle East
- Mycoplasma
- Oman
- PAP Smear
- Positive STI Results
- Qatar
- Saudi Arabia
- Sex Education
- Sexual Health
- Sexual Health News
- Sexually Transmitted Infections
- STD Symptoms
- STD Tests and Screens
- STI Results
- STI Treatment
- STIs
- Sustainability
- Swab Tests
- Syphilis
- Trichomoniasis
- Uncategorized
- United Arab Emirates
- Ureaplasma
- Urine Tests




